Today's newsletter is about a specific form of Large Sadness, while Friday is about Small Joys.
Missed the LIVE I did with two of my siblings, Kara and Eddie Stern? Fear not! You can watch it here. We talked about breathing and humming. We also laughed a lot and my phone kept crashing.

A bunch of years ago, during a therapy session, I mentioned that I’d been feeling a strain of sadness that wasn’t going away.
I wasn’t depressed—not exactly—and I also wasn’t sad in the traditional way, i.e., I wasn’t crying all the time. I wasn’t crying at all. What I felt was akin to un-feeling, not a deadness per se, but a flatness that, when I went toward it, made me realize that I was not doing as well as I thought.
I tried to explain the emotionless emotion, describing it as a low-grade monotony, as though the world inside and outside me were wallpapered in a boring sameness, lacking dimensionality. Imagine a persistently low hum that never oscillates or changes tone.

Getty Images | Oscar Wong
I couldn’t recall when it began, and I was struck with a sudden sharp realization that maybe I’ve been like this forever, and was only now just realizing that I was, at my core, a perennially sad human person.
In response to all this, my therapist said it sounded like “Dysthymia,” a word I’d never heard of. She explained that it’s a form of depression—it’s also referred to Persistent Depressive Disorder (I’ll refer to it as both names in this post), but it expresses itself differently than clinical depression. Rather, it’s got its own personality, and features that are distinct to the condition.
Dysthymia is a Greek word that means “bad state of mind.”
And, like depression, it can interfere with your daily life, which certifies it as a clinical disorder. But here’s the kicker: According to the DSM, depression is only diagnosable as a clinical disorder when a person experiences five or more symptoms in the same two-week window, while dysthymia is diagnosed as a clinical disorder when the sufferer has suffered for a period of TWO YEARS!!
Despite how unfamiliar many people are with the word “dysthymia,” it’s a fairly common complex mood disorder, and affects about 6% of the population.
And like so many other unpleasant things in this world, it mostly affects women and has a high incidence of comorbidity (meaning that more than one disease or disorder is present).
Symptoms

Getty Images | Doug Armand
The main features of dysthymia include lasting sadness, or as I had tried to describe it to my therapist, suffering from a mood that feels constantly “empty.” People with Persistent Depressive Disorder may have trouble concentrating and making decisions.
They have less energy and often feel fatigued. Similar to chronic depression, there is a sense of hopelessness that can interfere with a person’s hunger, causing them to either under- or overeat.
Sleep can be restless, or not come at all. Or, sleep can overwhelm a person, and wakefulness feels hard to come by.
At the same time, the dysthymic person will suffer from low self-esteem, and often be irritable, negative, or have pessimistic thoughts.
While the requirements are a bit different, children and adolescents can also suffer from Persistent Depressive Disorder (called Pediatric Persistent Depressive Disorder). If they’ve felt this way for a year, and are experiencing two or more of these symptoms, they may be suffering from dysthymia.
Cause

Getty Images | Holloway
While the cause of Persistent Depressive Disorder is not known, there are some biological and circumstantial factors that can contribute and increase your risk of developing PDD. These include (but are not limited to):
Issues of imbalances in brain circuitry. Research shows that changes in neurotransmitters and how they interact with the neural circuits involved in maintaining mood stability might be at play.
There may be physical changes in the brain from trauma
Stressful life events or trauma, such as the loss of a loved one or financial problems
a family history of the condition
a history of other mental health conditions, such as anxiety or bipolar disorder
chronic physical illness, such as heart disease or diabetes
drug use

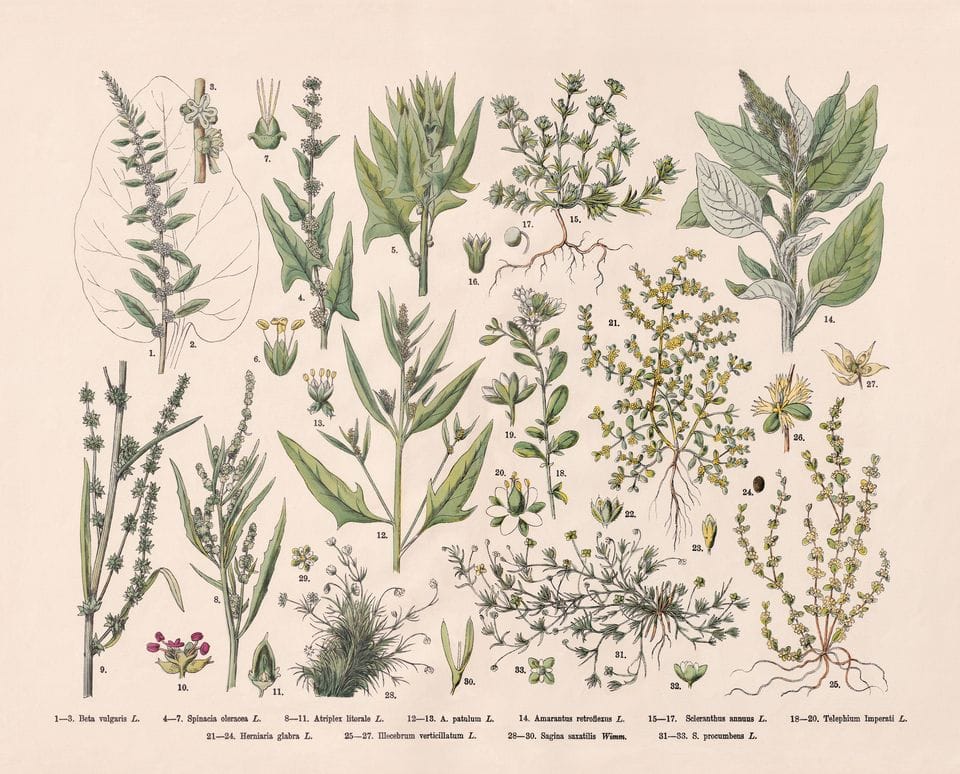
Original art for "How to Live" by Edwina White
Treatment
The typical treatment for dysthymia includes talk therapy and medication like Selective Serotonin Reuptake Inhibitors (SSRIs), Tricyclics, or Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Like most things related to mental health, you might need to try a few different medications and dosages before you experience relief. If you don’t have a therapist right now, try to find one who makes you feel safe and understands this disorder.
You might also want to consider doing Cognitive Behavioral Therapy (CBT), which works to help challenge and change your thinking and behavior patterns.
Naturally, these things cost money, and money, as we know, is hard to come by. So, if you’re unable to pay for a therapist, have a look at some of these resources that link to more affordable options.
A good therapist will help you cope with your emotions, adjust to change and challenges, identify your emotions, thoughts, and behavior patterns that trigger or exacerbate symptoms, help you swap out negative beliefs for more positive ones and set realistic goals for your mental, physical, and intellectual well-being.
It’s also important to adjust any lifestyle choices contributing to your sadness. We all know that exercise is helpful, but start slow; just take a one-minute walk and build from there.
Getty Images | ZU_09
Avoid weed, alcohol and too much coffee for a month and see if that helps. Look into slow-moving practices like meditation, qi-jong, tai-chi or yoga. And of course, eat your fruit and veggies. Having music on in the house is also helpful (according to me).
While symptoms must be present for at least two years before a diagnosis can be made, once caught, treating dysthymia can be effective and life enhancing.
That is the good news: dysthymia is conquerable. I’m proof that it can go away once it’s addressed. I am no longer dysthymic, although I admit there are days when I feel a waft or two of that same sadness, but I’m able to catch it and say,
“No thanks, I’ll pass.”
Obviously that doesn’t always work, but it does help hammer home the point that I have more control over my feelings and emotions than any disorder wants me to believe.
And the same goes for you.
You got this.
Had you heard of Dysthymia before this? Have you ever suffered from it?
Let me know in the comments!
Until next week I remain…
Amanda
(Nope, I'm not a therapist or medical professional. I'm just a human being who has spent most of her life trying to figure out how to live.)
Anything bought in the How to Live Bookshop can earn me a small commission, which goes to subsidize this newsletter.
📬 Email me at: [email protected]
📖 Buy my book Little Panic: Dispatches from an Anxious Life

